(Circulation. 1997;96:2102-2112.)
© 1997 American Heart Association, Inc.
A Reappraisal of Mouth-to-Mouth Ventilation
During Bystander-Initiated Cardiopulmonary Resuscitation
A Statement for Healthcare Professionals
From the Ventilation Working Group of the Basic Life Support and Pediatric Life
Support Subcommittees, American Heart Association
Lance B. Becker, MD, Chair;
Robert A. Berg, MD; Paul E. Pepe, MD,
Key Words: AHA
Medical/Scientific Statements • death, sudden • cardiopulmonary resuscitation •
ventilation
Introduction
Cardiopulmonary resuscitation (CPR) performed by bystanders clearly
improves survival and victims of out-of-hospital cardiac arrest and
other life-threatening conditions such as drowning and respiratory
arrest.1
2
However, despite three decades of promulgation, CPR is not performed
for the majority of victims who require lifesaving care.3
4
5
6
Studies have identified reticence to perform mouth-to-mouth
ventilation as a significant barrier to more frequent performance of
bystander CPR.1
7
8
9
10
11
12
13
In addition to acting as a barrier to initiation of CPR, the
mouth-to-mouth ventilation component of CPR may have other adverse
effects, such as promoting gastric insufflation14
15
16
17
or decreasing the percentage of time allocated to effective chest
compression.18
19
20
Because early CPR plays a central role in
saving lives, the Ventilation Working Group of the Basic Life
Support (
Historical Rationale for
Mouth-to-Mouth Ventilation
Historical Studies of Ventilation
The importance of ventilation during resuscitation has been accepted for
centuries, with the earliest descriptions of assisted ventilation documented
in stories of the prophets Elijah and Elisha in the Bible. Examples
of mouth-to-mouth ventilation and the suggestion to teach it widely
to the public also exist in a description of the resuscitation of a
miner overcome by smoke in 1744.21
Experiments conducted in 1796 demonstrated that expired air was
"safe for breathing."22
23
Over the next two centuries various artificial ventilatory
techniques were tested during resuscitation, including the use of
bellows, rolling the victim over a barrel, or positioning the victim
on a trotting horse. Perhaps the most commonly used and effective
artificial ventilation techniques were those that were popular both
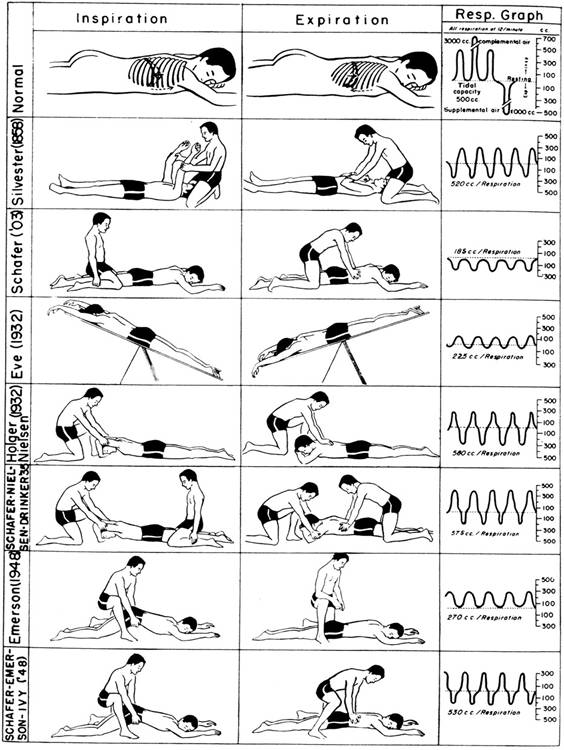
in the ![]() ). With many of these
techniques the patient was placed in a prone position (perhaps
favoring an open airway); pressure was then rhythmically applied to
and released from the posterior chest and back while the patient's
arms were lifted cyclically. By 1953 at least 105 published articles
described methods for artificial resuscitation of adults; 12
articles discussed resuscitation of children.25
During the first half of the 20th century these so-called
"manual" techniques were endorsed and taught by the Red
Cross and commonly used by lifeguards, the military, and Boy Scouts.
). With many of these
techniques the patient was placed in a prone position (perhaps
favoring an open airway); pressure was then rhythmically applied to
and released from the posterior chest and back while the patient's
arms were lifted cyclically. By 1953 at least 105 published articles
described methods for artificial resuscitation of adults; 12
articles discussed resuscitation of children.25
During the first half of the 20th century these so-called
"manual" techniques were endorsed and taught by the Red
Cross and commonly used by lifeguards, the military, and Boy Scouts.
Figure 1. Manual techniques of artificial respiration. There
was intense interest in artificial ventilation methods during the first half of
the 20th century. From Gordon et al.24
Copyright 1950 American Medical Association.
In a landmark study in the 1950s, Safar and
colleagues26
demonstrated that the tongue and soft palate commonly obstructed the
upper airway in unconscious persons. They further demonstrated that
the manual ventilation techniques developed in the 1900s were relatively
ineffective in the presence of such obstruction. The chin-lift and
jaw-thrust
techniques for opening the airway of
the supine patient were developed to remove obstructions and
maintain airway patency.27
28
Safar and colleagues29
30
then demonstrated a practical advantage of expired breath ventilation
over previous manual methods with the patient lying supine. Specifically
they compared tidal volumes generated during mouth-to-mouth (or
mouth-to-airway) ventilation with those generated using the older
manual techniques in paralyzed and anesthetized adults with normal
circulation. Although the Holger-Nielsen method (one of the most
effective manual techniques) generated >340 mL/min tidal volume
in five of six patients, it was still less effective than
mouth-to-mouth ventilation (Fig 1![]() ). On the basis of
these and similar confirmatory studies, mouth-to-mouth ventilation became
the therapy of choice for out-of-hospital respiratory arrest by the
1960s.31
32
). On the basis of
these and similar confirmatory studies, mouth-to-mouth ventilation became
the therapy of choice for out-of-hospital respiratory arrest by the
1960s.31
32
While these studies on ventilatory
techniques were being conducted, other laboratories sought a
practical method of providing circulatory support during cardiac
arrest. Because external chest compression could provide partial
circulatory support, the mouth-to-mouth ventilation technique was
added to chest compression to create modern CPR. The "ABC"
sequence of resuscitation—Airway patency, Breathing
(with mouth-to-mouth ventilation), and Circulation (chest
compression)—emerged as a practical and empirical means of CPR (Fig
2![]() ).33
34
Because most adult cardiac arrest victims become apneic or generate
abnormally diminished respiratory efforts, it has long been assumed that
mouth-to-mouth ventilation should be an integral component of CPR.
On the basis of the physiological principle of rapidly restoring
"normal" breathing and circulation and the subsequent
success of CPR in the clinical setting, a sequence of mouth-to-mouth
ventilation at a rate of 10 to 12 breaths per minute for adults,
with each breath followed by five chest compressions (two rescuers),
was recommended by consensus and adopted by the AHA.1
35
).33
34
Because most adult cardiac arrest victims become apneic or generate
abnormally diminished respiratory efforts, it has long been assumed that
mouth-to-mouth ventilation should be an integral component of CPR.
On the basis of the physiological principle of rapidly restoring
"normal" breathing and circulation and the subsequent
success of CPR in the clinical setting, a sequence of mouth-to-mouth
ventilation at a rate of 10 to 12 breaths per minute for adults,
with each breath followed by five chest compressions (two rescuers),
was recommended by consensus and adopted by the AHA.1
35
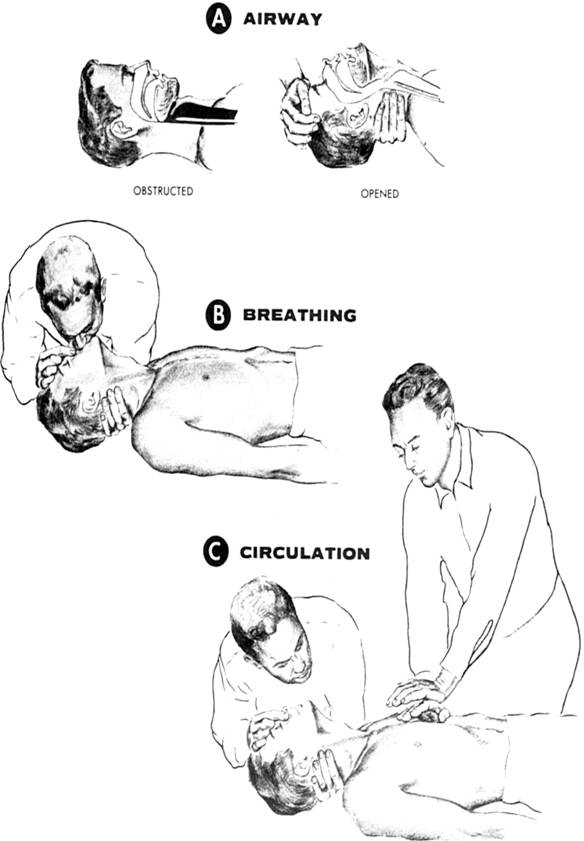
Figure 2. The ABCs of resuscitation. Modern CPR was a combination of
ventilatory support with circulatory support. From the Cardiopulmonary Resuscitation
Committee.34
Copyright 1966 American Medical Association.
Effectiveness of Traditional
Techniques of Cardiopulmonary Resuscitation
Over the past 25 years many studies have reinforced the empirical practice
of the ABC sequence for CPR by confirming the effectiveness of
bystander-initiated CPR.2
4
5
36
37
38
39
The outcome of most cases of adult cardiac arrest depends primarily
on the time interval from cardiac arrest until defibrillation.5
40
41
42
43
44
Therefore, rapid provision of defibrillation is considered the most
important determinant of successful outcome.1
40
41
43
44
However, traditional CPR extends the time available for successful
defibrillation and resuscitation.43
44
Specifically investigations of "adult" type cardiac arrest
in laboratory animals indicate that (1) maintenance of adequate
coronary perfusion pressure and resultant myocardial blood flow
during chest compression are critical for optimal survival and (2)
the window for successful bridging until defibrillation is 10 to 18
minutes.45
46
47
48
49
50
51
52
53
Clinical studies similarly indicate that success of CPR improves
when (1) the cardiac arrest is witnessed, (2) immediate bystander
CPR is provided, (3) adequate coronary perfusion pressures are
obtained during CPR, (4) the initial rhythm is ventricular fibrillation, and
(5) early defibrillation is provided.5
36
40
41
42
43
44
54
55
56
57
58
59
60
61
Data from both animals and humans concur: time is of the essence.
Traditional bystander-initiated CPR can improve survival when it is
started within 4 to 6 minutes from the time of collapse and followed
with advanced cardiac life support within 10 to 12 minutes of
collapse.43
44
Nevertheless, although these studies have reinforced the value of
the ABC technique, few studies have focused on the relative efficacy
of mouth-to-mouth ventilation or chest compression alone.
Does Assisted Ventilation Improve Outcome of Cardiopulmonary
Resuscitation?
Respiratory Physiology During
Cardiopulmonary Resuscitation
Pulmonary function involves both oxygenation (diffusion of O2 into
the bloodstream) and ventilation (movement of a volume of gas in and
out of the lungs, resulting in removal of CO2). Although
the roles of ventilation and oxygenation are intertwined during
breathing, each has important, separate considerations in patient
management. Inadequate oxygenation of the blood (ie, hypoxemia) can
occur during CPR, due to hypoventilation (high arteriolar PCO2),
pulmonary alveolar shunting, and ventilation-perfusion mismatch.
These physiological abnormalities may be the result of lung
deflation, frank atelectasis, pulmonary edema, airway obstruction, or
pulmonary aspiration of gastric contents before or during CPR.
Supplemental oxygen administration and recruitment of lung volume
through reinflation are the mainstays of therapy for hypoxemia in
these circumstances. Endotracheal intubation is often necessary for
reinflation, particularly in view of diminished lung compliance after
several minutes of apnea and chest compression.62
63
64
65
Traditionally the ventilatory goals of CPR
training techniques have stressed empirically that minute
ventilation be more or less normal.34
However, current techniques for mouth-to-mouth ventilation were
developed in paralyzed anesthetized subjects with normal circulation,
conditions not typically present during CPR scenarios. Both
oxygenation and ventilation requirements may be altered during
circulatory arrest because cardiac output and pulmonary blood flow
generated even during CPR that is well performed are far lower than
blood flow during spontaneous circulation. With low blood flow,
end-organ tissues become ischemic, extract a higher percentage of O2,
and accumulate higher levels of CO2 ("tissue
acidosis"),66
67
but arterial blood gases may not reflect these tissue conditions.68
As a result, the goals of oxygenation and ventilation during CPR
have not been established, and interpretation of arterial blood
gases is not clear.68
69
Therefore, it is difficult to evaluate current oxygenation/ventilation
techniques. Collectively there is little evidence that oxygenation and
ventilation need to be "normalized" during fibrillatory cardiac
arrest because the primary disorder is due to low blood flow, not respiratory
insufficiency.
Sources of Ventilation During
Cardiopulmonary Resuscitation
Although active mouth-to-mouth ventilation has been stressed in traditional
CPR training, it is also important to consider that many other
sources of gas movement can contribute to oxygenation and
ventilation in patients receiving CPR. Indeed, there are several
potentially important sources of ventilation during cardiac arrest
with attempted resuscitation including compression-induced ventilation
and gasping respiration. Compression-induced ventilation commonly
results when gas is expelled from the lungs and is "passively
inhaled" following elastic recoil of the chest wall during the
relaxation phase.70
71
72
73
74
75
76
In multiple animal studies, compression-induced ventilation alone
has proved quite substantial when measured.71
74
75
76
77
However, measured minute ventilation and arterial oxy-genation
decrease after 4 to 10 minutes of CPR with or without assisted
ventilation, possibly because of progressive chest
compression–induced atelectasis and thoracic deformity.71
78
Thus, with longer periods of cardiac arrest, ventilation may become
more important. This is supported by animal studies in which chest
compression periods were more prolonged, demonstrating that chest
compression with assisted ventilation and adequate lung inflation
result in better oxygenation compared with chest compression without
assisted ventilation.71
74
In addition to compression-induced ventilation, spontaneous
respiration, usually in the form of agonal or gasping breathing,
commonly occurs during cardiac arrest in both animals and humans,
further contributing to total ventilation.75
76
78
79
Several recent investigations in animals have specifically established
that spontaneous gasping occurs early during CPR and is associated
with a better outcome.74
75
76
78
79
Spontaneous gasping may simply reflect improved oxygen delivery to
the medulla during CPR, or it may reflect a shorter cardiac arrest
interval. However, the mechanics of gasping may also improve the
effectiveness of CPR because of (1) improved venous return during
the negative-pressure inspiratory efforts, (2) augmentation of
cardiac output due to increased intrathoracic pressure during the
expiratory phase of gasping, and (3) improved pulmonary gas exchange
due to both increased airflow and the more physiological
"pulling open" of those dependent lung zones subject to
deflation. In one study of swine, spontaneous gasping contributed
approximately half of the measured minute ventilation during
chest-compression-only CPR, compared with <10% during chest
compression plus mechanical ventilation.74
Therefore, in human and animal studies some
component of compression-induced ventilation and gasping
respiration—which by themselves may be important sources of gas exchange—is
present unless specifically prevented. In turn, studies reporting
CPR performed "without ventilation" may not be strictly
accurate; the authors more likely mean "without mouth-to-mouth
ventilation" or "without assisted ventilation."
Although not necessarily measured or reported, the contributions of
compression-induced ventilation and gasping respiration may still be
substantial in the absence of mouth-to-mouth ventilation. In
contrast to the original studies of mouth-to-mouth ventilation in
which anesthetic and paralytic agents were administered to subjects
with normal circulation, these components of ventilation during CPR
may be sufficient for a short time to produce survival when coupled
with effective chest compression.
Experimental Studies of Assisted
Ventilation
With the recognition that ventilatory requirements during cardiac arrest are
unclear and acknowledging that compression-induced ventilation and
gasping respiration may be important sources of gas movement, the
requirement for and timing of mouth-to-mouth ventilation can be
questioned. A canine study on the effects of mechanically assisted breathing
(as an approximation of human mouth-to-mouth ventilation) was
performed in 1983 by Meursing et al.80
In this study CPR was delayed for 5 minutes following sudden
circulatory arrest, and no significant fall in arterial PO2 or rise in PCO2 was
observed. Chest compression was then initiated, but assisted ventilation
was withheld for 2 minutes. No significant fall in arterial PO2 or rise in PCO2 was
demonstrated over the next 30 seconds. This study, reported only in
an abstract, was a key consideration in CPR guidelines developed in
the
Many laboratory studies support this
concept. Berg and colleagues82
demonstrated that fibrillatory cardiac arrest in swine provided with
chest compression alone for 9.5 minutes maintained an arterial pH of
7.33 and arterial PCO2 of 48
mm Hg. In a nonintubated canine cardiac arrest model, Chandra et al70
demonstrated that arterial oxygen saturation could be maintained
above 90% with a measured minute ventilation of 5 L/min being
generated during the fourth minute of chest compression alone
without any assisted ventilation.
The need for assisted ventilation during CPR
for fibrillatory arrest has been evaluated in four swine studies
with long-term survival. Each reported nearly identical 24-hour
survival and neurological outcome with chest compression alone
versus chest compression plus assisted ventilation.74
75
76
82
Fibrillatory cardiac arrest intervals varied from 30 seconds to 5
minutes, and CPR was provided for 8 to 12 minutes. In a more recent
study swine underwent a 5-minute fibrillatory cardiac arrest interval,
followed by 8 minutes of (1) chest compression alone, (2) chest compression
plus assisted ventilation, or (3) no CPR at all. Assisted
ventilation (at 15 mL/kg tidal volume) was provided with 17% oxygen
and 4% carbon dioxide to better simulate the exhaled gas delivered
during human mouth-to-mouth ventilation. The results showed that
without CPR there were no survivors. Both the
chest-compression-alone group and the
chest-compression-plus-assisted-ventilation group had significantly
better survival than the no-CPR group. However, whether or not
assisted ventilation was performed made no detectable difference on
either return of spontaneous circulation or 24-hour survival rates
(Fig 3![]() ).76
).76
|
Idris and colleagues83
have demonstrated that with prolonged arrest intervals beyond 6
minutes, supplemental oxygenation and assisted ventilation should
still be considered critical determinants of CPR success. In one
study, swine underwent 6 minutes of untreated ventricular
fibrillation, followed by 10 minutes of chest compression plus
assisted ventilation (12 mL/kg) with 85% oxygen versus chest
compression without assisted ventilation. The nonventilated animals
were paralyzed to prevent gasping and its effect on total
ventilation. Return of spontaneous circulation was achieved in 9 of
12 (75%) ventilated animals versus only 1 of 12 (8%, P<.002)
nonventilated animals. However, with arrest intervals of less than 6
minutes, these differences were not apparent. The investigators
further demonstrated that assisted ventilation with either hypoxic
or hypercarbic gas admixtures during CPR resulted in lower
resuscitation rates compared with assisted ventilation with 85%
oxygen.84
In summary the published experimental data
on animals collectively suggest that assisted ventilation may not be
critical in the early minutes after onset of sudden fibrillatory
cardiac arrest if adequate chest compression is provided. However,
after relatively longer intervals of untreated fibrillatory cardiac
arrest, some form of ventilatory support is likely to become
critical for successful resuscitation outcomes. Whether
mouth-to-mouth ventilation as the form of ventilatory support is
helpful during even prolonged fibrillatory cardiac arrest remains
unclear.
Clinical Studies of Mouth-to-Mouth
Ventilation
Are the results obtained from animal studies applicable to CPR in
human beings? Upper airway anatomy of animals differs from that of
human beings; thus, upper airway obstruction during cardiac arrest
may differ among species. Many animal species demonstrate frequent
and prolonged gasping. Laboratory animals also do not have coronary
artery disease. Unlike animal studies, the adequacy of oxygenation
and ventilation during chest-compression-only CPR (ie, without
mouth-to-mouth ventilation) has not yet been demonstrated in human
beings receiving CPR.
Nevertheless, the available human data to
date are consistent with findings in animals.38
75
85
86
For example, Weil et al86
demonstrated that during the first few minutes of CPR in humans, arterial
pH, PaCO2, and
bicarbonate change little from prearrest values. In addition, agonal
respiration or gasping has also been documented in 40% of 445
out-of-hospital cardiac arrest victims and 55% of those victims with
witnessed arrests.85
Furthermore, as in animal studies, agonal respiration or gasping was
associated with improved survival. Survival was 27% when gasping was
present, compared with 9% when it was not. It is uncertain if the
gasping was a marker for better central nervous system perfusion or
shorter arrest intervals or if the agonal breaths themselves
contributed to improved outcome.
Notably, recent investigations in humans
with the active compression-decompression CPR device (plunger type)
demonstrated that excellent minute ventilation (>6 L/min) was
maintained in four cardiac arrest victims without assisted
ventilation or intubation of the airway.87
New investigations are still necessary to determine whether standard
chest compression consistently results in adequate gas exchange for
successful resuscitation of human victims of cardiac arrest.
Although physiological studies are
informative, long-term survival in the clinical setting is the major
therapeutic end point of CPR. The Belgian Cerebral Resuscitation
Group38
39
prospectively evaluated 3053 out-of-hospital arrests. Physicians on
the ambulances evaluated the quality of bystander CPR for
compression and ventilation. Long-term survival of those treated
with good-quality chest compression alone and those treated with
good-quality chest compression plus mouth-to-mouth ventilation was
comparable (15% and 16%, respectively) (Fig 4![]() ). Survival when either
of these techniques was used was significantly superior to survival
without any CPR (6%, P<.001). The data confirm that
bystander CPR can be lifesaving but also suggest that mouth-to-mouth
ventilation may not be necessary for survival of cardiac arrest, at
least during the immediate moments after arrest. The authors of the
study cautioned that conclusions drawn from these observations should
be limited to adult patients with witnessed fibrillatory cardiac
arrest.
). Survival when either
of these techniques was used was significantly superior to survival
without any CPR (6%, P<.001). The data confirm that
bystander CPR can be lifesaving but also suggest that mouth-to-mouth
ventilation may not be necessary for survival of cardiac arrest, at
least during the immediate moments after arrest. The authors of the
study cautioned that conclusions drawn from these observations should
be limited to adult patients with witnessed fibrillatory cardiac
arrest.
|
Lengthier periods of arrest may require
earlier ventilatory support. The observation that some ventilatory
interventions are helpful after prolonged fibrillatory cardiac
arrest may indicate an oxygenation or lung inflation requirement as
much as a need for ventilation (CO2 elimination). It
seems probable that progressive lung deflation and airway closure
occurs during chest compression without gasping or mouth-to-mouth
ventilation. Such lung deflation will lead to increased pulmonary
shunting and progressive hypoxemia. Reversal of lung deflation with
an occasional lung inflation may be the critical pulmonary
intervention to prevent hypoxia. If so, it may still be unnecessary
to "normalize" respiratory rates in fibrillatory cardiac
arrest until spontaneous circulation returns. Future studies should
therefore attempt to delineate the critical timing, tidal volumes,
and rates for optimal resuscitation.
Are There Adverse Effects of Mouth-to-Mouth Ventilation?
Respiratory Effects
When no endotracheal tube is in place, assisted ventilation maneuvers often
are associated with gastric insufflation and pulmonary aspiration of
gastric contents, which in turn may cause adult respiratory distress
syndrome, pneumonitis, and possible death.63
Some studies suggest a 10% to 35% incidence of pulmonary aspiration of
gastric contents associated with CPR. During mouth-to-mouth ventilation,
positive pressure in the oropharynx forces air into the lungs. Gas,
however, flows down the path of least resistance, which may be
either the trachea and lungs or the esophagus and stomach. Gastric
insufflation is more apt to occur when (1) pulmonary compliance
decreases (eg, with CPR, pulmonary edema, atelectasis, obesity, and
the supine position), (2) airway resistance increases (eg,
obstructive pulmonary disease), or (3) lower esophageal sphincter
tone decreases.14
15
88
89
Lower esophageal sphincter tone usually
prevents regurgitation of gastric contents and provides resistance
to gastric air flow during positive pressure ventilation. The normal
esophageal sphincter opening pressure is about 20 to 25 cm H2O.90
91
However, this energy-dependent muscular tone decreases rather
quickly after circulatory arrest. In a swine model of CPR, mean
esophageal sphincter opening pressure decreased from 20.6 cm H2O
before cardiac arrest to 5.6 cm H2O after 5 minutes of
cardiac arrest.92
In anesthetized patients with adequate circulation, gastric insufflation
commonly occurs with bag-valve mask ventilation unless cricoid pressure
is provided.93
During cardiac arrest and CPR, pulmonary compliance decreases,
increased inspiratory pressures may be needed to inflate the lung,
and lower esophageal sphincter tone may decrease, all factors that
increase gastric insufflation. Regurgitation was noted to occur
primarily after the stomach was insufflated with air.16
Not surprisingly, in one series gastric insufflation and pulmonary
aspiration were documented in nearly half of cardiac arrest victims
after CPR with mouth-to-mouth ventilation.17
Another consideration is whether there are
important differences between exhaled gas and ambient air. While
room air has 21% O2 and 0.03% CO2, exhaled gas
was observed to contain a mean O2 concentration of 16.6%
to 17.8% and a mean CO2 concentration of 3.5% to 4.1% during
one- and two-rescuer CPR.19
Thus, as provided during mouth-to-mouth ventilation, expired gas is
slightly hypoxic and contains considerably more CO2 than
ambient air ventilation achieved with gasping and compression-induced
ventilation alone.94
Although expired gas rescue breathing is
safe and may be life-saving for patients with respiratory arrests,
the hypercarbia may have adverse cardiovascular effects when
compared with ambient air ventilation during circulatory arrest. In
one study of isolated hypercarbia, animals ventilated (12 mL/kg)
with 95% O2 and 5% CO2 did as poorly as
animals receiving no assisted ventilation at all during CPR.84
Another investigation showed that swine ventilated with room air
during 6 minutes of CPR had a rate of successful resuscitation (83%)
twice that of animals ventilated with simulated exhaled gas
ventilation when both groups received similar tidal volumes (38%, P<.01).95
Consistent with animal studies are cellular studies that demonstrate
modest increases in concentration of CO2 can inhibit the
rate and force of cardiac contraction, suggesting that elevated CO2
has a direct cardiodepressive effect.96
97
Circulatory Effects
Obviously a single rescuer performing CPR on an adult or child cannot
provide chest compression and mouth-to-mouth ventilation simultaneously. Thus,
it follows that with more time spent attempting ventilation, less
time will likely be allocated to chest compression and vice versa.
As noted, successful resuscitation has been highly correlated with
the timing and degree of restored myocardial blood flow and coronary
perfusion pressure, which are in turn dependent on the effective
provision of chest compression of a sufficient rate and depth.98
99
100
101
Therefore, time spent attempting ventilation may take away valuable
coronary perfusion. In support of this concept are recent studies
that suggest that when rescuers attempt ventilation using current
AHA recommendations, the compression rate and depth become
inadequate.102
Current AHA guidelines for adult CPR recommend a chest compression
rate of 80 to 100 per minute and a respiratory rate of approximately
12 breaths per minute, with compression/ventilation ratios of 15:2
with one rescuer and 5:1 with two rescuers. However, achieving these
recommended guidelines in the real world has been demonstrated as
problematic for both one- and two-rescuer adult CPR with mouth-to-mouth
ventilation.18
19
20
101
102
103
One study of in-hospital two-rescuer CPR found that only 2 of 12
rescuers gave 80 compressions or more per minute,103
whereas another investigation of simulated two-rescuer CPR on a
manikin found that compression rates averaged 75 per minute and that
the depth of compression was inadequate in 14% to 22%.101
These inadequacies of chest compression observed in two-rescuer CPR
appear to be even worse in studies of one-rescuer CPR.18
19
20
In a study of healthcare professionals performing one-rescuer CPR on
a manikin, only 15% achieved a rate of 80 compressions per minute
despite continuous coaching.19
Further investigation confirmed that even immediately after
successful completion of a basic CPR course, compression rates were
particularly inadequate; on average, only 56 compressions per minute
were provided by the 129 medical students studied.20
These data suggest that the competition
between time for ventilation and time for compression during
one-rescuer CPR is a "zero-sum" game; time spent on
ventilation takes precious time away from chest compression and
support of myocardial blood flow. It is surprising that this aspect
of CPR as practiced in the real world (ie, cycle time spent on
ventilation versus cycle time spent on compression) has not been
studied. It is worrisome that multiple studies have demonstrated
survival rates to be consistently correlated with coronary perfusion
pressure whereas no studies of fibrillatory arrest have shown
improved rates of survival with early ventilation. Future studies
need to take these real-world factors into account and not assume
that performance of CPR is in complete adherence with AHA guidelines
(which appears to be infrequently achieved).
Does Mouth-to-Mouth Ventilation
Inhibit Performance of Bystander Cardiopulmonary Resuscitation?
Despite widespread acknowledgment of its value and efficacy, CPR is
not performed by bystanders in the majority of cases for which it is
indicated. Furthermore, several recent studies have documented a
lower overall frequency of bystander CPR performance compared with
earlier investigations.3
Although this latter finding may have several possible explanations
(including the failure of the medical community and public health
officials to effectively teach the public the skills of CPR), the
perceived risk of disease transmission during CPR, even by
healthcare workers, has become increasingly suspect as a major
factor.
The actual risks of disease transmission
during mouth-to-mouth ventilation are quite small. There are
isolated reports of possible transmission of Helibacter pylori,104
Mycobacterium tuberculosis,105
meningococcus,106
herpes simplex,107
108
109
shigella,110
streptococcus,111
and salmonella.112
No reports on transmission of HIV can be found. Nevertheless,
despite the remote chances of its occurring, fears regarding disease
transmission are common in the current era of universal precautions.
Indeed, not only laypersons but physicians, nurses, and even
Fear of disease transmission may not be the
only reason that mouth-to-mouth ventilation inhibits bystanders from
initiating CPR. When mouth-to-mouth ventilation is combined with
chest compression, the CPR technique becomes a complex psychomotor
task that can be difficult to teach, learn, remember, and perform.82
114
Educational principles suggest that a simpler technique, such as
chest compression without mouth-to-mouth ventilation, would be far
easier to teach the public. If it were known that the use of chest
compression alone was nearly as efficacious as when combined with
mouth-to-mouth ventilation, potential rescuers might start
chest-compression CPR faster and more frequently because it is
easier to perform in an actual emergency. In addition, the greater
ease of learning, retaining, and performing such a simple procedure
could lead to more widespread performance of bystander CPR, thereby
improving survival rates for victims of cardiac arrest.
Special Considerations:
Implications for Future Guidelines
It is important to emphasize that this report makes no changes in
current AHA CPR guidelines and to consider why no changes are
warranted. To summarize, during fibrillatory cardiac arrest, mouth-to-mouth
ventilation may provide a modest therapeutic advantage over chest
compression alone, and it may have some deleterious effects. Both experimental
and very limited clinical studies to date suggest that mouth-to-mouth
ventilation may be deferred for several minutes in the patient with
sudden fibrillatory arrest. No studies on mouth-to-mouth ventilation
are yet available for asphyxial cardiac arrest. On the basis of this
review, in the most applicable clinical scenario for delaying
mouth-to-mouth ventilation, an adult (older than 40 years) suddenly
collapses from ventricular fibrillation. The collapse is witnessed
by a bystander who can immediately initiate chest compression.
However, this is a limited subpopulation of cardiopulmonary arrests
and is not applicable to many resuscitations, such as those
conducted for children, victims of submersion, respiratory failure,
and many other arrest types. In addition, the available data from
laboratory animals also suggest that after several minutes of
fibrillatory arrest some form of ventilation is helpful, presumably
to reinflate collapsing gas exchange units and prevent profound
hypoxia. Therefore, it is important for future studies to delineate
the specific circumstances and time limits under which mouth-to-mouth
ventilation might be deferred. Without these data, rational
guidelines cannot be provided. Although the current data are
insufficient to warrant a change in CPR guidelines and training,
they are compelling enough to recommend additional experimental and
human trials to better delineate what the exact role of
mouth-to-mouth ventilation should be during CPR.
It is also important to note that the
current discussion and available research focus only on the
contribution of mouth-to-mouth ventilation in the setting of sudden
adult fibrillatory cardiac arrest. The potential application of
mouth-to-mouth ventilation may be much broader than merely
responding to fibrillatory arrest. Intuitively, mouth-to-mouth
ventilation seems clearly indicated in cases of cardiopulmonary
arrest associated with airway obstruction, water submersion, or
preceding respiratory symptoms. Likewise, in children and young
adults, respiratory compromise, not cardiac arrest, is the more
common threat to life; thus, respiratory management should not be
deferred. Submersion and respiratory problems are the typical
precipitating causes of nontraumatic cardiac arrest in pediatric
patients and young adults.6
115
116
In addition, a child's pulse may be difficult to locate and measure.117
118
119
120
These children may only be hypotensive (or even normotensive), and
ventilatory support from mouth-to-mouth ventilation seems the
highest priority under these circumstances.
Although the above recommendation on
usefulness of mouth-to-mouth ventilation during asphyxial arrest for
children with respiratory failure is logical, not even this is
supported by data comparing the effectiveness of mouth-to-mouth
ventilation with chest compression alone. A large amount of research
is needed before the role and timing of mouth-to-mouth ventilation
can be better clarified. As in adults, the relative importance of
mouth-to-mouth ventilation and prompt defibrillation may be quite
different among the many subgroups of cardiac arrest victims.121
Unfortunately, as with adults, in the majority of pediatric
out-of-hospital arrest patients, basic bystander CPR is not attempted.
The working group continues to recommend prompt ventilatory support
in the form of mouth-to-mouth ventilation for apneic, pulseless,
unresponsive children.
Conclusions
and Recommendations
Traditional bystander CPR with chest compression and mouth-to-mouth ventilation
has been documented to save lives. Nevertheless, CPR is not being
performed in the majority of cases for which it is needed. As a
result, an alarming number of premature deaths occur each year in
the United States alone due to failure to provide basic CPR.1
Requiring that mouth-to-mouth ventilation be an essential component
of one-rescuer CPR has added to the complexity of teaching,
learning, remembering, and performing this procedure. Provision of
mouth-to-mouth ventilation has important potential disadvantages, including
gastric insufflation and less cycle time spent on effective chest
compression. Above all, aesthetic and infectious disease concerns by
the public and healthcare providers appear to be major barriers to
provision of basic CPR.
Although it seems possible that
mouth-to-mouth ventilation is not needed during the first minutes of
sudden witnessed circulatory arrest with suspected ventricular fibrillation,
it is likely that mouth-to-mouth ventilation should be the initial
intervention for arrest of suspected respiratory etiology. If a
delay in mouth-to-mouth ventilation is being considered, the overall
net impact on the public for saving lives from all causes of arrest,
not merely sudden fibrillatory circulatory arrest, must also be
taken into account. Updated guidelines on CPR are published at
regular intervals. It is the hope of the working group that additional
data will be available for consideration at the international conferences
on CPR planned for the year 2000.
The working group recommends that
- Current guidelines for performing mouth-to-mouth
ventilation during CPR should not be changed at this
time. Indeed, it should be noted that the current AHA guidelines
state that if a person is unwilling to perform mouth-to-mouth
ventilation, he or she should rapidly attempt
resuscitation, omitting mouth-to-mouth ventilation.1
Clearly provision of chest compression without mouth-to-mouth
ventilation is far better than not attempting resuscitation
at all.38
- Additional research initiatives are required to
expressly delineate the role of mouth-to-mouth
ventilation in the management of sudden death. Such studies
on ventilation should evaluate the timing, rate, and depth
as well as conditions under which respiratory assistance should
be used. In addition to determining optimal CPR in the laboratory,
more research on real-world obstacles to learning, remembering,
and actually performing CPR should be evaluated and
incorporated into future recommendations.
- Clinical trials involving human subjects who receive
chest compression with or without mouth-to-mouth ventilation
are ethical and necessary to determine how to save the most
lives with basic CPR. Institutional review boards and national
agencies interested in public safety should be aware of the
limitations of current data to adequately justify current practice
guidelines. Well-designed studies that answer important questions
on CPR should be encouraged.
- Organizations and agencies interested in public safety
and reduction of premature death should allocate
resources for research on these high-yield issues that
will determine future CPR guidelines. Unlike many areas of
medicine, the design and methods to find definitive answers
to these questions are readily available and merely await financial
support for completion.
|
|
Footnotes |
"A Reappraisal of Mouth-to-Mouth Ventilation During Bystander-Initiated
Cardiopulmonary Resuscitation" was approved by the American Heart
Association Science Advisory and Coordinating Committee in July
1997.
This article also appears in Annals of
Emergency Medicine (November 1997), Journal of Respiratory
Care (September 1997), and Resuscitation.
A single reprint is available after
September 30, 1997 by calling 800-242-8721 (US only) or writing the
American Heart Association, Public Information, 7272 Greenville
Avenue, Dallas, TX 75231-4596. Ask for reprint No. 71-0118. To
purchase additional reprints: up to 999 copies, call 800-611-6083
(US only) or fax 413-665-2671; 1000 or more copies, call
214-706-1466, fax 214-691-6342, or
© 1997 American Heart
Association, Inc.